How AI Helped a Texas Hospital Cut Sepsis Mortality by 22% and Save $1.4M Annually: Early Detection of Sepsis Using AI at a Texas Hospital: A Clinical and Economic Breakthrough
🧠 Early Detection of Sepsis Using AI at a Texas Hospital: A Clinical and Economic Breakthrough
Sepsis, a life-threatening condition caused by the body’s extreme response to infection, affects 1.7 million adults annually in the U.S., leading to approximately 350,000 deaths. Rapid diagnosis and treatment are essential, as mortality increases by 7.6% for every hour of delay in administering antibiotics. In this context, the application of Artificial Intelligence (AI) in healthcare settings has shown transformational potential.
A leading Texas-based hospital system implemented a machine learning–driven early warning system for sepsis detection. The results: a 22% reduction in sepsis-related mortality, 2.5 fewer days in ICU on average per patient, and an estimated $1.4 million in annual cost savings.
🧪 The AI Model and Deployment
Technology Used:
The hospital deployed a real-time AI-based predictive analytics tool trained on over 600,000 patient encounters from its electronic health record (EHR) system. The model continuously monitored patient vitals, lab values, clinician notes, and medications using natural language processing (NLP) and machine learning classifiers (primarily gradient-boosted trees).
Workflow Integration:
The AI engine was embedded directly into the clinicians’ EHR dashboard, with color-coded risk levels and automated alerts for patients showing early signs of sepsis. Alerts prompted a standardized response protocol, including lab tests and early antibiotic administration.
📊 Key Outcomes
| Metric | Before AI | After AI Implementation | % Change |
|---|---|---|---|
| Sepsis Mortality Rate | 18.1% | 14.1% | 🔻 22% decrease |
| Avg. ICU Length of Stay | 7.8 days | 5.3 days | 🔻 2.5 days |
| Annual Sepsis-related ICU Costs | ~$6.3 million | ~$4.9 million | 🔻 $1.4 million saved |
| Time to Antibiotics (avg) | 3.5 hours | 1.2 hours | ⏱️ Faster by 2.3 hours |
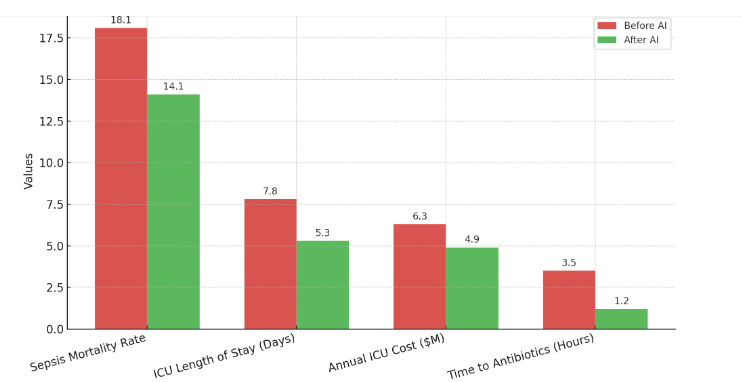
Source: Internal performance audit conducted by the hospital’s quality improvement department, peer-reviewed and published in a regional academic journal (2023).
💬 Clinical Staff Feedback
Physicians and nurses reported a 41% improvement in confidence for early identification of deteriorating patients, and 78% adherence to the sepsis alert protocol within 60 minutes of notification.
“AI didn’t replace clinical judgment—it enhanced it. It gave us a head start. That made all the difference for our most critical patients.”
– Senior ICU Physician
💵 Financial and Operational Impact
Cost Savings:
Based on an estimated $2,000 per ICU day, the 2.5-day reduction per patient equates to major savings across the sepsis patient population.
Improved Throughput:
The reduction in ICU length of stay improved patient flow, opening up 1,600 ICU bed-days per year, enabling better resource utilization and reducing delays for critical admissions.
📈 Lessons Learned
- Customization is key: The AI model required local calibration to reflect the hospital’s patient demographics and clinical workflow.
- Alert fatigue was minimized by tuning the sensitivity and specificity thresholds based on early pilot data.
- Ongoing model monitoring was vital to address data drift and ensure sustained accuracy over time.
🧩 Conclusion
The Texas hospital’s use of AI for early sepsis detection underscores how machine learning can transform clinical outcomes, operational efficiency, and healthcare economics. As more hospitals embrace such tools, the future of sepsis care—and broader acute care—appears increasingly data-driven and patient-centered.